Kate Bowler: Hi, I’m Kate Bowler, and this is Everything Happens.
K.B.: Look, the world loves us when we are good, better, best. But this is a podcast for when you want to stop feeling guilty that you’re not living your best life now. We’re not always doing mountain top yoga. I used to have my own delusion of living my best life now. I’m a Duke professor, wine and cheese enthusiast, wife and mom. Instagram gold. Then I was diagnosed with Stage 4 cancer. That was four years ago and I’m still here. And now I get it. Life is a chronic condition. The self-help and wellness industry will try to tell you that you can always fix your life. Eat this and you won’t get sick, lose this weight and you’ll never be lonely. Believe with your whole heart and God will provide. Keep this attitude and the money is yours. But I’m here to look into your gorgeous eyes and say, hey, there are some things you can fix and some things you can’t and it’s OK that life isn’t always better. We can find beauty and meaning and truth. But there’s no cure to being human. So let’s be friends on that journey. Let’s be human together.
Kate Bowler: Today, we’re talking about agency. Agency is this word I use a lot. It describes the degree to which a person has the ability to make decisions about their life, to change it, control it, direct it. We all want a little bit of agency, especially when we’re facing impossible circumstances. Sometimes it feels like we have unlimited agency. There is that Churchill quote that says “We are still masters of our fate. We are still captains of our souls.” That is the feeling of unlimited agency, unlimited possibility. But then there are those of us who have been crushed by disease or had our lives upended by loss or mental illness has ravaged our families. Agency seems harder to come by, especially now when we are all facing the uncertainty of a pandemic with no clear end in sight. We lose a little bit of our ability to know how to act when we feel like we are spinning our wheels. Or worse, buried deeper and deeper in the mud. Some people see an obstacle and bulldoze their way through it. Others are simply bulldozed. What makes the difference?
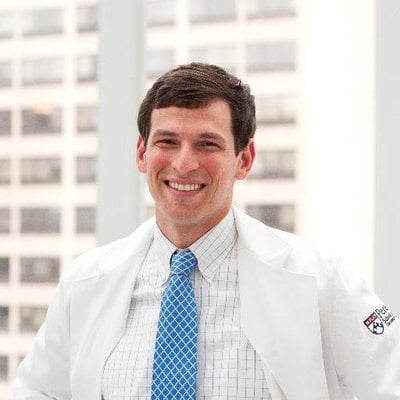
Today, I’m speaking with a human bulldozer. His name is David Fajgenbaum. David is an incredible super achiever. He has two master’s degrees and an M.D. from UPenn and he’s only 34.
I know that the road to all those accomplishments hasn’t been easy. When he was in medical school, his body was ravaged by a mysterious illness, taking him to the brink of death more times than anyone should remember. But he is the author of Chasing My Cure because in the midst of all that, he found the cure to his own disease. But we’ll get to that soon. David, hello. I’m so glad we’re speaking today.
David Fajgenbaum: Kate, I’m so happy to be chatting with you as well.
K.B.: I love hearing all about your life because it feels like you’ve lived a thousand lives. I say you have had so many aspirations. You played quarterback at Georgetown. You had a gorgeous girlfriend. Your life was on this trajectory of success and endless possibility. But then when you were 19, your mom got really sick. Can you tell me what happened?
D.F.: So just as you said, I was a couple weeks at Georgetown at that time. I had just gone off to college and I received the news from my dad that was just totally devastating. And that was that my mom was diagnosed with a terminal brain tumor. And it just totally, as you can imagine, just totally upended my life. And I went from this, I guess young and optimistic and energetic football player who kind of had one view for the world to being so devastated by my mom’s diagnosis.
K.B.: Did it change your view of what you felt was possible after you knew that, like, something that awful could happen to someone you love so very much?
D.F.: It did. It was tough for me, because not only was it something so bad happening to someone I love so much, but it was someone who is just so good. And everything about her. It’s just she lived for other people. She was basically an agent for good. That’s who she was and what she did. And so that was really hard for me.
K.B.: It does sound like her very, like her, hospitality, like her amazing generosity is something you inherited, though, because I just I see how you immediately take what you do and like make it a gift for other people.
D.F.: Well, thank you. She definitely taught me that we really have a responsibility to do what we can in the time that we have. I don’t know if it was inherited or if it was just that I got to watch the ultimate giver, you know, day in and day out for 18 and a half years of my life that it’s definitely been instilled in me. She was an amazing person. And even after her passing, I just felt like I needed to continue her legacy in some way. And so I started an organization in her memory called AMF. My mom’s name was Ann Marie Fajgenbaum and we named this group AMF after her initials. And it stood for Ailing Mothers and Fathers. And now it stands for Actively Moving Forward. It’s a support network for college students dealing with illness or death of a loved one. And I think it’s really the ultimate embodiment of her. It’s connecting young people who are having a hard time with other young people to be shoulders to lean on.
K.B.: Wait, you went from being like a 19 year old human, Tigger, who played quarterback to like opening a grief network.
D.F.: For me, my life just went from football, football, football to grief support. And I just want to be a cancer doctor because I want to treat people like my mom.
K.B.: Yeah, maybe because I don’t know that many unbelievably athletic people, David. But like I saw the photos when you were like superhuman giant football man. And you’re like such an incredible dichotomy of what you experience next because you’re you’re like winning bench press competitions and like you’re working out all the time then and then you start to have these mysterious symptoms. And I I’d love to hear, like how you first understood what was happening to you and where you thought that might take you.
D.F.: Over the course of just a couple of weeks. I went from being totally healthy, like you said, literally winning bench press contests to feeling more tired than I’ve ever felt before, noticing pooling in my ankles, noticing lumps in my neck that I didn’t know what they were at the time. And yeah, I got really, really, really sick. I was so sick that at the time I finally went to the emergency department, I really wanted to take this one medical school exam because I because I guess I don’t know, I’m crazy. I guess I really wanted to make it through this exam and then then I’d go get checked out. So I kind of limped from my medical school exam down the hall to the emergency department and they ran a series of tests and they said, “David, your liver, your kidneys, your bone marrow and your lungs are shutting down. We have to hospital you right away.” And within a couple of days, I got critically ill. I had a retinal hemorrhage that made me blind in my left eye. I gained 70 pounds of fluid due to my liver and kidney failure, and I needed a feeding tube and basically required daily transfusions to keep me alive, all with no diagnosis.
K.B.: You and your loved ones actively prepared for your death. What happened?
D.F.: Kate, it was 11 weeks of just kind of pain and fear and suffering and just reflection in the hours that I would be awake during the day, I would reflect on my life because I I knew that I was not going to survive and the doctors knew that I would not either. And actually at one point when I was really at my sickest 11 weeks in, the doctors told my family that they should say goodbyes. I don’t remember too much of that experience because I was so sick. But I do remember reflecting back on my life and thinking about what I had done, what I hadn’t done. And I remember that the things that I regretted actually had nothing to do with things that I did do. What I really regretted were the things I didn’t do or I didn’t say. And in particular what I didn’t say to to my prior girlfriend, Caitlin. We had dated for a couple of years from college and had broken up about six months before I got sick. And I specifically remember not fighting for our relationship and saying to myself, well, it’s okay we’re twenty five years old, we’ve all the time in the world. If it’s meant to be, it’s meant to be. And then there I was on my deathbed, having my last rites read to me and realizing that that I would not have more time and that I wish I spent those last six months with Caitlin and that I wished that I could have a life with her and that we could have a family one day and just being totally devastated.
K.B.: Yeah, yeah, yeah. Yeah, that makes sense to me. There’s like a difference. The loss of potentiality is like such a big and intense loss, like not in the abstract, but right when you’re picturing someone that you would never be sick of.
D.F.: You might be sick of me at some point, but I would never be, that’s right.
K.B.: I know it’s totally dumb, but there’s this line in a movie I love where like someone just said, oh, what I would have given to have tired of you. And like, I felt that, too, when I was having my hospital moment where I was just like looking at my husband and thinking about my kid and thinking like I would give anything to get really, really sick of you.
D.F.: And he’s pretty awesome, I know Toban. I can see why you would say that.
K.B.: Yeah, I imagine that must’ve been so hard to toggle both like the medical side of your brain. You’re such an incredible synthetic mind. And then to be simultaneously processing all the personal loss and then just the helplessness of being a patient.
D.F.: And even worse, what was I think may be most difficult for me was that the medical system that I had bought into and I was halfway through my medical training was also helpless and was also unable to identify a diagnosis. But thankfully, right around actually within 48 hours of having my last rites read to me, the diagnosis was finally made of Idiopathic Multicentric Castleman disease. And because we know so little about the disease, the only treatment at the time was chemotherapy. And so I was given immediate chemotherapy with the hope that it would be kind of a last ditch effort to save me. And thankfully it did. And thankfully, about a month later, I was able to walk out of the hospital at Duke.
K.B.: Yeah, even when things were absolutely awful, joy still crept in. What would you say to someone who is not sure that it’s okay to laugh?
D.F.: My dad and I decided to take a walk around the hematology oncology floor at this hospital and it was late that night on New Year’s, and we passed by a gentleman who had been clearly drinking on New Year’s Eve. He was like swinging in his chair, in the family waiting area. And then our next lap around, we saw that he had fallen onto the ground. And so my dad ran over to him and helped him back into his chair. And he looked at my dad and I should mention that I was carrying an I.V. pole with me and I had a huge belly because I was in kidney failure. And I was bald from the chemo. And he looked at my dad and I and he said, “thanks so much. Good luck to you and your wife.” And then I looked at my belly and I realized he thought I was my dad’s pregnant wife. And we laughed so hard Kate. I mean, I like almost fell on the floor I was laughing so hard. I turned to my dad and I said “hey you better hug your wife” and we just were like, floored. And I think that it’s those sort of moments where, you know, I was getting misgendered as my father’s wife. Like, there’s a lot of reasons that could have been particularly complicated. But I was so happy to be alive. And we just laughed so hard. And I think that during really tough times, not to say that there’s always, like, you know, something to laugh about, because truly there are some times where there was nothing to laugh about. And you know this all too well. There are times you can you can do is cry. But I think there are these times in between where it feels like the only thing there is to do is to cry. And I probably could have cried, you know, when I got confused as my dad’s pregnant wife. But I think that sometimes if you can find some positivity and some humor in it, at least for me, that that made me feel connected to my family.
K.B.: Yeah, totally, but also alternate theory. You’d make a beautiful woman. So I think. I think both possibilities are open. I’ll make sure there’s photos of you in the show notes. So people can just kind of weigh in on that. Don’t worry, I’ll send you the results.
K.B.: I’m just thinking of how intense it must have been to finally have some more language around your diagnosis, but then start to realize that that didn’t mean that there was a cure.
D.F.: After the first six months of being sick, the first thing I did was reach out to Caitlin and to try to get back together with her and to tell her that, you know me taking, me disbelieving that it would work out at some point in the future was just the wrong approach in that and that I wanted us to be together. And it was such an important priority. And thankfully, she felt the same way. So Caitlin and I were dating again. And I told my dad, my sisters and Caitlin, I’m gonna dedicate the rest of my life to trying to identify treatments and maybe a cure for this disease. And I remember the look in their eyes they obviously they gave me kind of like a half smile, like, you know, you got it Dave. You know, we believe in you. But they were just so terrified as to whether I would make it through the next day.
K.B.: It sounds like it was like a whole family, all hands on deck kind of thing. Am I remembering it right that at one point your dad was like having a regular phone call with the director of the National Institute of Health?
D.F.: Yes, it was Tony Fauci, who, of course, everyone now knows. And the best part about this Kate is, so my dad got Tony Fauci’s cell phone number from a family friend. And the assumption was that maybe my dad would call Dr. Fauci maybe, maybe once, you know, given the story. By the way, you would love my dad. He’s got it. He’s like the most extroverted person in the world. And he is a bulldozer for sure. And he’s not a very eloquent bulldozer. And so he would call Dr. Fauci every day for three weeks while I was in the ICU. And he didn’t know that it was Dr. Fauci. He just knew it was some guy named Foochi. So my dad would say, Hey, Foochi, and he would just run through all the lab tests and the clinical features. And he would he would go through every day and update. And Tony Fauci would spend 30 to 45 minutes on the phone with my dad every day for three weeks while I was in the ICU. My dad never called the doctor, my dad never knew who he was. And I got out of the hospital literally months later. And I was like, Dad, I have this memory of this like Foochi, what is Foochi? And he was like, oh, yeah, I was calling this guy named Foochi at the NIH. I don’t know who he is. And so I like Google Foochi like f o o c h i. And google corrects me as Tony Fouchi and then corrects me further and I learn that he has a Presidential Medal of Freedom. And I was like, Oh, my gosh Dad you’ve been calling Tony Fauci. And he was like, oh yeah, that sounds right. Oh, my gosh. And so.
K.B.: I love that for so many reasons. Partly it’s also explaining you to me right now.
D.F.: A little bit. Yes.
K.B.: I’m so glad you talked about those moments of intense uncertainty because that’s, I know a lot of people who listen to this podcast, have either experienced a lot of uncertainty themselves or they are used to standing with those who do. Were you just, where, there’s really actually no ground to stand on. And if you don’t mind, I’d like to read a passage about how you described experiencing that, where no one is actually standing there with you, not even your doctors. You write: I knew the language the doctors use, the careful truth-telling, the hedging, the open endedness. I’ve spoken that language before. Now that it was directed at me, it didn’t feel nearly as careful or open ended as I’d once assumed. Instead, the words felt like they were casting me out of the room, out of the hospital entirely. I’d been consigned to the plane of possibility. Anything was possible because no one knew. I was on my own.
K.B.: That’s so beautifully put. That is like world without landmarks anywhere. That sounds exactly right.
D.F.: And it was so terrifying. And I think that you know this all too well, Kate, that we just want answers from our doctors. We want, we want to know with certainty, you know, percentages at that point in my journey where I wrote that passage. It was where I was sitting in my hospital room and I was actively dying for the fourth time. And I was so sick. And that’s when, I’d been on this experimental drug before, before this relapse. So clearly, the drug wasn’t working. And I was asking all the right questions to my doctor. You know, what else is there out there? What sort of leads are there? Who’s working on things? They were all the ones that I should have asked earlier, but I was too afraid to ask because I didn’t want to actually know the answer. I wanted to pretend that there must be other drugs. I wanted to pretend that there must be promising research. And I’d kind of put those things out of my mind. But then when that drug no longer worked, I needed to now find out what else was there. And my doctor just kept saying, no one knows. And it was no one knows to information about the disease. But it was also was that, no, there are no more drugs in development. And it was absolutely terrifying.
K.B.: Yeah, I’m just kind of blown away, though, by your by your gut instinct to like like step forward. Like no matter what, you just like, you push in. Because I know you cycled through this unreal move from life to death to life to death till like almost dying over and over and over again until like all all the while realizing that there is no there’s no cure or adequate treatment in the works to save someone like you. And you write: I couldn’t accept living in between almost dying. Unbelievable. Like, you just decide that, like, you’re going to get to work.
D.F.: If I’m going to survive, I need to find, I need to basically create knowledge that doesn’t exist today. And I wasn’t foolish in thinking that, like I could do it. In fact, I didn’t think that I could do it. I mean, A -I didn’t want to I wanted there to be a solution. I was kind of like, oh, my gosh, I wish I didn’t have to do this and too it was, I’m not going to do it. In all likelihood, I am not going to find anything that’s going to help me or help anyone else. But if I don’t try, then I know what my outcome’s going to be. My chance is maybe less than 1 percent. But, you know. But you’re telling me there’s a chance is basically the way that I was looking at it. And so then I just dove in full speed.
K.B.: David, I don’t mean for this to sound flippant any way, but when you say “so, you’re saying I have a chance?” does that also remind you of the Dumb and Dumber moment?
D.F.: I was 100% referring to Dumb and Dumber. And I wasn’t sure if you were going to pick up on that what’s going to be um.
K.B.: That’s so funny because like when reading your book, you know, we’ve had dinner and like, I just absolutely adore you and I’ve been thinking about your unbelievable capacity for hope. And I literally wrote down here the moment in Dumb and Dumber when like one character is being rejected by a woman who says “so the chance of us ending up together are” and I quote “one in a million”, to which he replies breathlessly. “So you’re saying I have a shot?” And it struck me honestly while I was preparing for this interview that you really talk about hope in the same way. You look at insane odds. And you seem to always say, “so, you’re saying I have a shot”.
D.F.: I mean, I don’t think I’ve ever made the total connection to that in Dumb and Dumber, but Dumb and Dumber might actually be an appropriate way to describe my outlook on odds and on chances. And I think it was from my experience with my mom and knowing that that I couldn’t just hope and I couldn’t just pray. I would need to hope, I would need to pray and I would need to act. And I think so often in life there’s this kind of it’s either or it’s either you hope and pray, or you take action. And I think that I think they need to come together. They need to work in parallel. We need to reflect on what we pray for because whatever we’re praying for, that means it’s really important to us. And often times we have the agency and the power to actually be a part of of making that which we’re praying for become a reality.
K.B.: Yeah, yeah, yeah. I like that. I like that. I I. I know that I flip flop sometimes between feeling like hyper agency. So like an inflated sense of what I can do. And that’s mostly just out of fear or hyper passivity because I’m overwhelmed. I’ve had too many choices. I’m tired. You know, it’s hard to to carve out that that place in the middle you’re describing where we can move forward faithfully. But we also know how to account for our circumstances. We don’t just assume things have to work out just because especially when the stakes are so high. I mean, you’ve just had this so many times in your life where all the best things are worth fighting for. And the decision either gets made for you or there’s only a small chance. And I’m, I think it’s especially knowing how much you lost with your mom that I’m just I’m so blown away that you decided that that you’d be a person of hope. It’s really it’s really spectacular.
D.F.: Oh, thank you.
K.B.: So you studied and wrote papers and developed collaborative research that ultimately led to you discovering the cure for your disease. What the hell, David? That wasn’t a question. Well, just what the hell?
D.F.: So. So, yes, I’m I’m literally alive and talking to you today, thanks to a drug that had never been used before for my disease that I was able to identify from research I did in my lab and thanks to this amazing collaborative network of people.
K.B.: So can you talk to me about the logistics of how you found the medicine that has kept you alive right now? Something you call it drug repurposing.
D.F.: There are 7000 diseases that don’t have any drugs and there are 15 hundred drugs that are approved for other conditions. And many of those fifteen hundred drugs may actually be able to work in the seven thousand diseases without any answers. And I’m a living example of one of those. So you basically take a drug that had an initial purpose and then you repurpose it and use it in another in another disease. And that’s an approach that I think is probably our greatest opportunity for many rare diseases. It’s unlikely that a drug company is going to develop a new drug for every one of the seven thousand rare diseases. It’s a lot more likely that some of those drugs that are already approved might actually also be able to help diseases without solutions. And so that’s something we’ve been been pushing for. You know, about 50 percent of patients now can benefit from the two drugs that I’ve been a part of identifying. And we’ve identified now a third drug that we’re hopeful is gonna help the other 50 percent of patients. But but there’s still work to be done. At the very beginning of my journey, I was okay with no agency. And then I kept fighting. I want more and more agency. I want more more control. I want to be held. And then the final decision that I had to make, do I take this drug or not? I wanted to punt it to someone else Kate. I didn’t want to have to be the one to make that decision, because there’s something really nice about when your doctor walks in and she says, this is the drug we’re going to give you and then you’re gonna get better and then we’re going do this scan. And then if something changes, we’re gonna give you this. And when she gives you that sort of a plan, you say, yes, this is what I’m looking for.
K.B.: Yeah, that’s my plan.
D.F.: There’s something so scary about saying, wait, I can’t like look at someone else’s diplomas and feel confident that they’re gonna make the decision. I’m making the decision today. And what if I got this wrong? What if my interpretation of this one experimental result is incorrect? And then it becomes so hard to to make a decision like that. And sometimes it can be paralyzing. But Caitlin and the prospect of of just making it to our wedding day wasn’t some sort of grand plan we’re going to live forever together. But just that prospect was enough to give me the courage to make the decision.
K.B.: Yeah, that sounds right, David. Like the feeling at some point, like we have agency, like we we have all the get up and go, but sometimes it’s love that can pull us toward the future or at least the possibility of imagining a future at all.
D.F.: You’re exactly right.
K.B.: I think it’s also a place of real hope, too, to give language to the fact that a lot of solutions to terrible and abiding pain are structural. You’ve been a champion of organization in which people had to put their minds and their institutions at work toward a common cause. And that’s, I think, probably an especially hopeful thing for people to imagine right now as we’re racing toward trying to solve all the variables around Covid 19, that like so much of our our own move toward the greater good are not just in our hope in heroic individuals, but in in heroic systems. And David, there’s stuff you’re doing in particular. So you’re applying things that you learned from your own research into Castlemans to further our global understanding of how to manage Covid 19. So like, what are you doing?
D.F.: I run a lab now at UPenn that’s focused on the immune system. I study Castleman disease, other immune system disorders. And also this concept of drug repurposing. And so I was driving down to North Carolina to to visit my sister and my brother in law. My brother in law has late stage A.L.S. and I haven’t gone to see him. And it was right before all of the Covid 19 challenges really arose here in the States. And it was late at night and Caitlin was asleep in the car. And I was driving down. It is kind of me on my own with my thoughts. And I remember I was driving and just thinking to myself, I just really hope. And I was also just yearning and praying and wishing that that some researchers out there would follow the approach that we’ve taken to Castleman Disease and would follow the steps. It’s kind of a very algorithmic way that we’ve gotten towards treatments for Castlemans. And I just hope someone does that. And then I kind of like snapped out of it. And I was like, wait a minute, why am I hoping that someone somewhere will do it? We just need to do it. This is like I’m here driving this car today because I stopped hoping that someone, somewhere would figure out Castleman disease. And it’s not easy. It’s not. I never wanted to try to figure out Castleman disease. And I don’t necessarily want to try to figure out Covid 19. I would love someone else to do that. That would be very nice. But it was kind of like, wait a minute. Like what? What have you been talking about for all this time? Why did you write this book about turning hope into action? That’s it’s literally the subtitle of my book, A Doctor’s Race to turn Hope into Action. And here I am just hoping that someone somewhere is going to do this. And so I felt really compelled. And since then, have have completely turned my lab of 13 scientists focused on Covid 19. And also the foundation that I run, the Castleman Disease Collaborative Network, we’ve repurposed and moved basically 20 volunteers towards Covid 19. So a team of about 30 of us have been racing after Covid 19 since I returned back to Philadelphia after visiting with my brother in law and sister.
K.B.: David, I’m so grateful we’re friends and I love knowing that at any moment you are out there turning hope into action. But let’s be real. I know we should all be right out there with you. Thanks so much for being here.
D.F.: Thank you so much Kate. And thank you for being a part of turning hope into action through your podcast, through inspiring people all the time, through sharing other people’s messages like this one. It really means the world to me.
K.B.: Thanks, friend
K.B.: David’s story is about hope, but what I heard sounded like two kinds of hope. Hope that doesn’t wait. Hope that anticipates and moves into the possibility of a beautiful future. Even when it may seem like a one in a million chance, it was hope with running shoes on. But he said something else I loved when he talked about his wife, Caitlin. He said just wanting to marry her made him hope. Seeing their wedding day months down the road gave him the courage to ask hard questions and to do something difficult and painful. In that moment, he was pulled into the future, pulled into hope by the sheer force of love. We are living in awful and uncertain times. And I know that hope feels like a strange word, but what David was calling us to was hilariously and wonderfully not to just sit around waiting for the cure we need. We need to look into our own lives and ask who is waiting on me to act? Who might be waiting on me to hope a little more? Maybe it’s your kid in the other room doing math right now. Maybe it’s your mom needing a Skype call, your patients or your customers as you step out the front door to encounter a scary world. But thank God for you when in acts big and small, you put your shoes on.
K.B.: This podcast wouldn’t be possible without the generosity of the Lilly Endowment. Huge thank you to my team: Jessica Richie, Keith Weston, Harriet Putman and JJ Dickinson. OK, but for real. Come be human with me. Find me on Instagram or Twitter at Katecbowler. This is Everything Happens with me, Kate Bowler.















Leave a Reply